End-stage renal disease, or kidney failure, affects between 4 and 7 million people worldwide (Lv and Zhang 2019) and over 750,000 people in the US alone (US Renal Data System 2019). Patients suffering from kidney failure require either ongoing dialysis treatment or a kidney transplant. Transplantation has been estimated to extend life relative to dialysis by between five and 10 years (Wolfe et al. 2008, 2009).
In the US, approximately 90% of patients who hope to receive a kidney transplant do not have access to a living donor and must participate in a centralised deceased-donor kidney allocation mechanism run by the Organ Procurement and Transplantation Network (United States Renal Data System 2019). However, deceased-donor kidneys are scarce: in 2019 there were almost 100,000 patients on the Network’s waiting list, but only 16,534 deceased-donor kidneys were transplanted that year.1
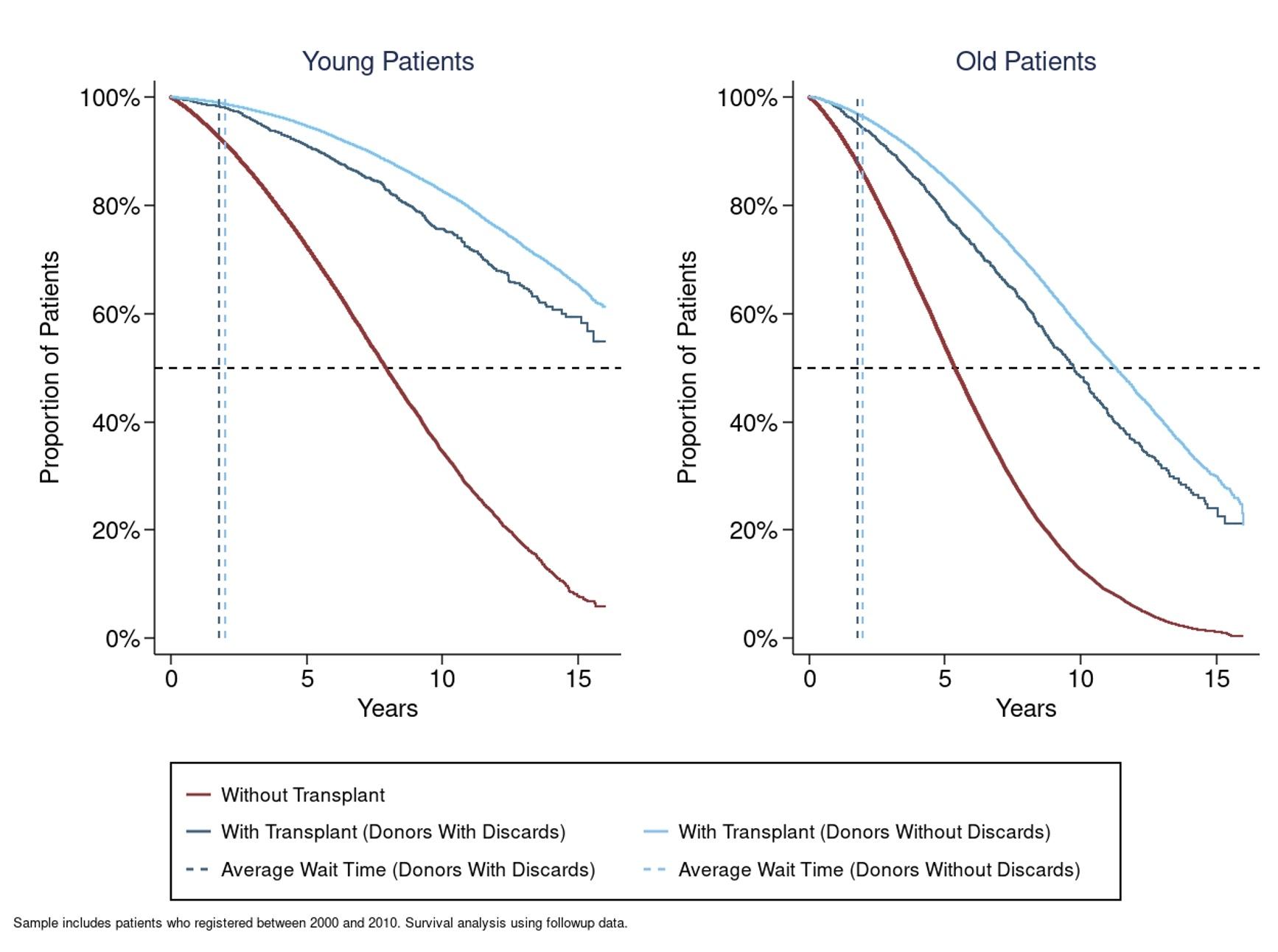
Figure 1 illustrates survival curves for old and young patients with and without transplants. The median young patient is projected to live for eight years without a transplant and over 15 years with a transplant, while the median old patient is projected to live for only six years without and around 12 years with a transplant.
Figure 1 Survival curves for young and old patients with/without transplants
Source: Agarwal et al. (2020)
In addition to their scarcity, the quality of deceased-donor kidneys varies substantially. The median old patient who is transplanted with a high-quality kidney is projected to live for about two years longer than the median older patient transplanted a low-quality kidney.
This heterogeneity in transplant quality depends on kidney-specific factors such as the age and health of the donor prior to death, as well as patient-donor specific factors, such as tissue compatibility. The total number of life years generated from transplantation therefore depends both on who is transplanted and the match between patient and donor.
Because of the scarcity and heterogeneity of deceased-donor kidneys, the allocation system plays an important role in determining whether we are making the best use of available organs. One important outcome is ‘life years from transplant’, a measure of the gain in life years from a transplant relative to dialysis (Wolfe et al.et al. 2008, 2009).
The question of how to achieve a kidney assignment that maximises life-year gains is an ongoing policy challenge. It is subject to equity and fairness constraints and the subject of recent academic research (Bertsimas et al.2013, Agarwal et.al. 2020), and policy discussion (Israni et al. 2014), including by the Organ Procurement and Transplantation Network kidney committee (Organ Procurement and Transplantation Network 2014).
The mechanism used to allocate deceased-donor kidneys combines a prioritised waiting list with patient choices to assign deceased-donor kidneys as they arrive. Kidneys are offered to patients sequentially, starting with the patient with the highest priority score, and patients can choose to accept or decline kidney offers. Patient priority is largely determined by waiting time but is also a function of patient and kidney characteristics. For instance, patients who are perfect tissue-type matches with the donor have high priority.
The Organ Procurement and Transplantation Network mechanism uses patient and donor characteristics to target transplants to specific patients, but also allows for patients to express their preferences through choice. Patient choice may help increase life years from transplant if patients and their doctors have specific knowledge about which kidneys are the best match, but it may also work against this policy objective. For example, choice could reduce average life years from transplant if doctors and patients have incorrect beliefs or if doctors’ incentives are misaligned. An important step in designing life-year maximizing mechanisms for kidney assignment is therefore determining the role of patient choice.
Evaluating life years from transplant from kidney assignments
In a recent study, we estimate the life years from transplant generated by the kidney assignment system using data on transplants and outcomes for patients on the deceased donor waiting list between 2000 and 2010 (Agarwal et al. 2020).2 Our approach measures how patient decisions and survival outcomes interact so that decisions may be correlated with life-year outcomes.
We find that patients are more likely to accept kidneys with higher expected life years from transplant. For example, patients are more likely to accept kidneys from donors who died of head trauma, which tend to generate more life years in the transplanted patient. This finding suggests that allowing for patient choice might improve average outcomes.
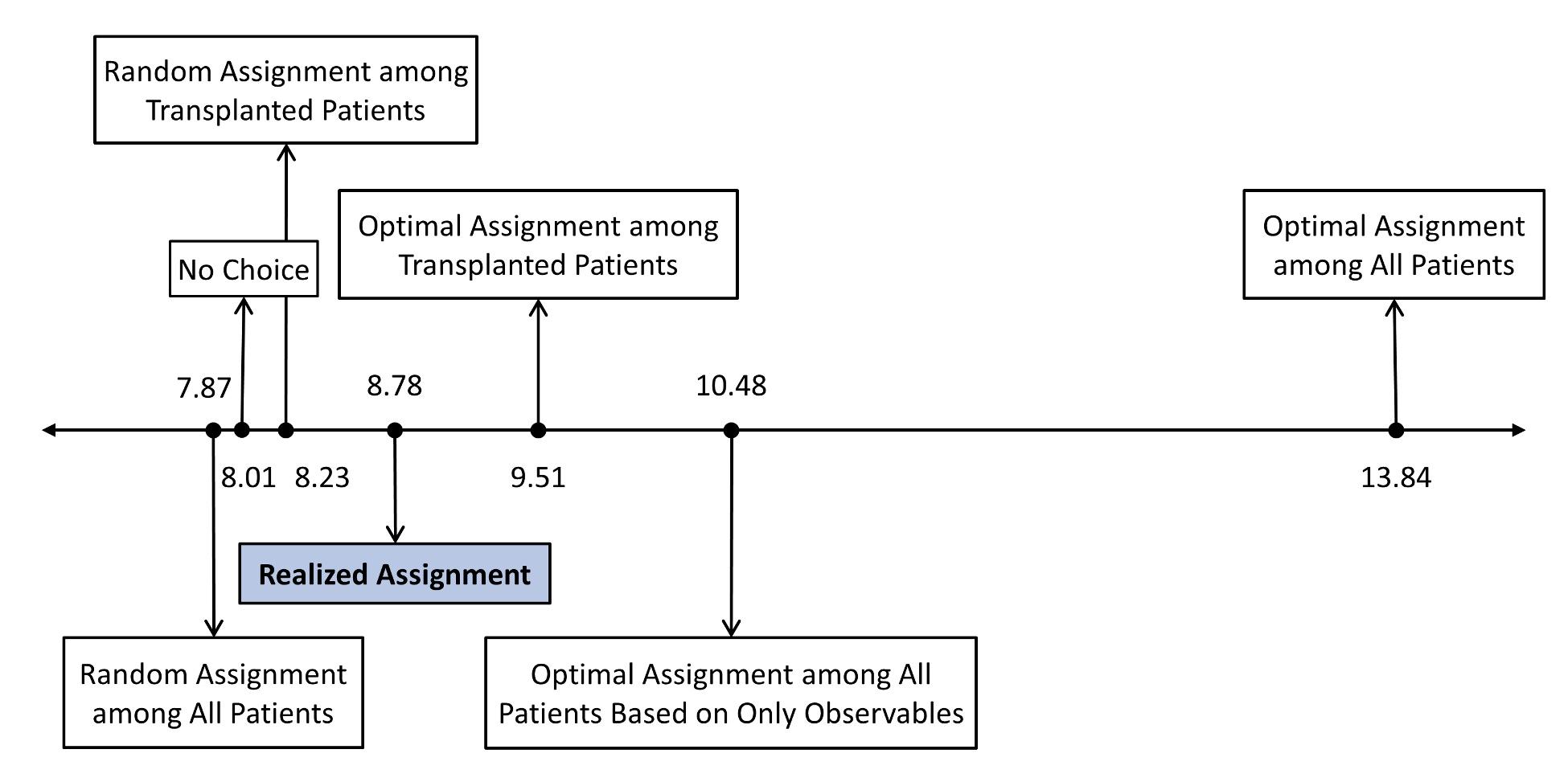
Although choice is beneficial, there is significant scope for further improvement. We use our model to compare the assignment system using alternative benchmarks. These results are illustrated in Figure 2.
Figure 2 Kidney assignment scenarios and estimated effect on life years from transplant
Notes: Comparison for patients and donors transplanted in 2005. Optimal assignment among all patients is calculated using all the relevant information about a patient’s prognosis prior to and after a transplant. For details about the assignments, see Agarwal et al. (2020).
- The median patient that received a transplant under the realised assignment is projected to live 8.78 years longer than they would have without a transplant. This figure is about one year longer than that achieved by a random allocation of kidneys to patients. Interestingly, this gain in life years is largely generated by patient choice. Simulations that use the mechanism’s priority rules alone to assign kidneys without allowing patient choice predict only marginally higher life years from transplant than the random allocation.
- Although the mechanism improves life-year gains relative to a random allocation, it is far from optimal. Our estimates suggest that an assignment that maximises life years from transplant could achieve a median life years from transplant of 13.84 years if all the relevant information about a patient’s prognosis prior to and after a transplant can be used. Such a system would allow the typical patient to live about five years longer than the life years generated by the existing assignment.
The planner’s dilemma
This potential improvement is not without roadblocks. There are at least two reasons why achieving the life-year-maximising assignment may not be desirable or feasible.
- First, we do not observe all the information that patients and doctors have about patient health and the quality of potential patient-kidney matches. A life-year-maximizing assignment that only uses patient and kidney characteristics currently reported to the waitlist mechanism achieves a median life years from transplant of 10.48 years. While lower than the theoretical maximum of 13.48 years, it is still about one and a half years longer than the life years from transplant achieved by the mechanism used by the Organ Procurement and Transplantation Network.
- Second, the five-year increase in life years over the realised allocation comes from a dramatic change in the set of patients that receive a transplant. Re-organising the allocation of kidneys without changing who is transplanted can only increase life years from transplant by about six months.
In particular, maximising life years from transplant requires transplanting younger and relatively healthier patients who would have lived longer without a transplant. It would result in the most urgently sick patients going without a transplant. This naturally raises important concerns because a life-year-maximizing allocation would result in younger, healthier patients receiving transplants at the expense of older, more urgently sick patients. Thus, the policy goal of improving life years from transplant conflicts with a moral imperative to transplant urgent cases.
The dilemma comes from the relationship between baseline health and determinants of life years from transplant that we estimate. We find that patients whose life would be extended the longest from a kidney transplant are also those who would live longer without a transplant. Moreover, life years from transplant primarily depends on the patient rather than patient-donor specific factors.
Indeed, concerns over equitable distribution of transplants have been concerns in past revisions of the assignment rules (Organ Procurement and Transplantation Network 2014). The fact that policymakers have some understanding of this tradeoff may explain why the Organ Procurement and Transplantation Network’s mechanism does not achieve the theoretical maximum life years from transplant of 13.84 years.
Our quantification of this tradeoff between equity and efficiency provides a starting point for the design of kidney allocation systems that explicitly maximise median life years from transplant subject to distributional constraints. This framework applies more broadly to the design of policies that assign scarce resources to maximise aggregate outcomes through non-market mechanisms. For instance, recent work has highlighted similar concerns in the design of distribution plans for the COVID-19 vaccine (Schmidt et al. 2020). Similar issues arise outside of healthcare. For instance, research highlighting complementarities between student ability and college quality (Dillon and Smith 2019) suggests that this tradeoff may also exist in the school-assignment context.
References
Agarwal, Nikhil, Itai Ashlagi, Michael A Rees, Paulo Somaini and Daniel Waldinger (2021), “Equilibrium allocations under alternative waitlist designs: Evidence from deceased donor kidneys”, Econometrica 89(1): 37–76.
Agarwal, Nikhil, Charles Hodgson and Paulo Somaini (2020), “Choices and outcomes in assignment mechanisms: The allocation of deceased donor kidneys”, working paper.
Bertsimas, Dimitris, Vivek Farias and Nikolaos Trichakis (2013), “Fairness, efficiency, and flexibility in organ allocation for kidney transplantation”, Operations Research 61(1): 73–87.
Dillon, Eleanor, and Jeffrey Smith (2019), “The consequences of academic match between students and colleges”, The Journal of Human Resources 55(3): 767–808.
Israni, Ajay K, Nicholas Salkowski, Sally Gustafson, Jon J Snyder, John J Friedewald, Richard N Formica, Xinyue Wang, Eugene Shteyn, Wida Cherikh, Darren Stewart, Ciara J Samana, Adrine Chung, Allyson Hart and Bertram L Kasiske (2014), “New national allocation policy for deceased donor kidneys in the US and possible effect on patient outcomes”, Journal of the American Society of Nephrology 25(8): 1842–48.
Lv, Ji-Cheng, and Lu-Xia Zhang (2019), “Prevalence and disease burden of chronic kidney disease”, Advances in Experimental Medicine and Biology 1165: 3–15.
Organ Procurement and Transplantation Network/UNOS Kidney Transplantation Committee (2014), “Report to the Board of Directors”.
Schmidt, Harald, Parag Pathak, Michelle Williams, Tayfun Somnez, M Utku Ünver and Lawrence Gostin (2020), “Rationing safe and effective COVID-19 vaccines: Allocating to states proportionate to population may undermine commitments to mitigating health disparities”, working paper.
United States Renal Data System (2018), “USRDS annual data report: Epidemiology of kidney disease in the US”.
Wolfe, R, K McCullough and A Leichtman (2009), “Predictability of survival models for waiting list and transplant patients: calculating LYFT”, American Journal of Transplantation 9(7): 1523–7.
Wolfe, R, K McCullough, D Schaubel, J Kalbfleisch, S Murray, M Stegall and A Leichtman (2008), “Calculating life years from transplant (LYFT): Methods for kidney and kidney-pancreas candidates”, American Journal of Transplantation 8(4 Pt 2): 997–1011.
Endnotes
1 Source: https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/
2 We analysed the assignment system in place prior to 2014 because long-run survival outcomes cannot be measured for the system put in place on December 2014.