Marijuana laws have been at the forefront of the policy debate in the US for decades as more and more states move to legalise the use of marijuana for medical and/or recreational purposes. By 2021, 36 states (along with the District of Columbia, or DC) had passed medical marijuana laws (MMLs), and 19 states (and DC) had passed recreational marijuana laws (RMLs). While debates on the legalisation of marijuana in the US are ongoing, it seems likely that MML and RML bills will be on the legislative agendas in several other states soon.
Insofar as marijuana legalisation affects marijuana use (Hollingsworth et al. 2022), legalising marijuana for both medical and recreational purposes can exert direct and indirect effects on individual outcomes and behaviours, and as such can have important public health consequences (Anderson and Rees forthcoming). In fact, there is vast evidence from the economic literature showing that legalising marijuana affects many factors, including traffic and workplace fatalities (Anderson et al. 2018, Hansen et al. 2020), risky behaviours such as increased sexual activities and reduced contraceptive use (Baggio et al. 2020), crime (Chu and Townsend 2019, Dragone et al. 2019), and labour supply (Nicholas and Maclean 2019).
Despite existing evidence of several unintended effects of marijuana legalisation, potential effects on mental health have received less attention from studies both in economics and public health. According to data from the Substance Abuse and Mental Health Services Administration, in 2020, 20.8% of American adults had a mental illness, with increasing associated economic costs for public finances.
Examining the mental health effects of marijuana legalisation jointly considering medical and recreational laws is important for the design of public policy, due to them having potentially different effects on individuals, while at the same time having complementary effects on wellbeing. On the one hand, medical marijuana legalisation could improve people’s wellbeing by treating existing health problems. On the other hand, recreational marijuana legalisation could lead to overuse and thus might negatively impact mental wellbeing.
As several studies show, these policies lead to increased marijuana use, therefore, it is possible that they have both direct and indirect effects on mental health. Use of cannabinoids can improve sleep quality and reduce stress disorder (National Academies et al. 2017), and evidence from the medical literature suggests that the former acts as an antidepressant (Bambico et al. 2007), therefore directly affecting mental health distress. On the other hand, marijuana use can also indirectly lead to adverse effects for younger people, as also argued in past Vox columns (Williams and van Ours 2009, van Ours and Palali 2013), by interfering with brain development, which continues until age 25 (Chadwick et al. 2013). In addition, these effects can be heterogeneous across the age distribution and type of legislation. Although marijuana use might produce harmful effects on young adults, for older people – who are less vulnerable to potential negative side-effects related to brain development and more likely to use marijuana as a medical treatment – the benefit of marijuana use might overcome potential negative side-effects, producing null or even positive effects. At the same time, marijuana legalisation could also affect mental health indirectly, depending on whether marijuana substitutes or complements other substances. Most studies point to marijuana and alcohol being substitutes (Crost and Guerrero 2012, Kelly and Rasul 2014), therefore, given the evidence that alcohol use increases suicide risk (Carpenter and Dobkin 2009), MMLs and RMLs might affect mental health also indirectly.
In a recent paper (Borbely et al. 2022), we examine the causal effects of marijuana legalisation on mental health, considering both medical and recreational marijuana laws and exploiting the staggered rollout of these policies across US states. In our study, we rely on two standard measures of mental health – the number of bad mental health days in the past 30 days; and the Kessler Psychological Distress Scale (K6), which is comprised of a series of six survey questions related to mental distress – from nationally representative survey data sets. To establish the main channel through which marijuana legalisation can affect mental health outcomes, we first examine the effects of marijuana laws on marijuana use and find evidence of a clear positive effect.
Institutional background
The US provides an interesting context as different states implemented these legislations at different points in time, thus allowing us to leverage variation in the timing of the rollout while at the same time controlling for other factors that are constant over time but might differ at the state level, and thus can interfere with the effect of the legislation on mental health. California was the first state to pass legislation to permit the use of medical marijuana in 1996. Several other states then followed suit and by 2021, 36 states had legalised marijuana for medical purposes. By 2021, legalisation of marijuana for recreational purposes has been introduced in 19 states; these laws were always passed in states that in earlier years had legalised marijuana for medical purposes.
Effects differ across age groups and by pre-existing health conditions
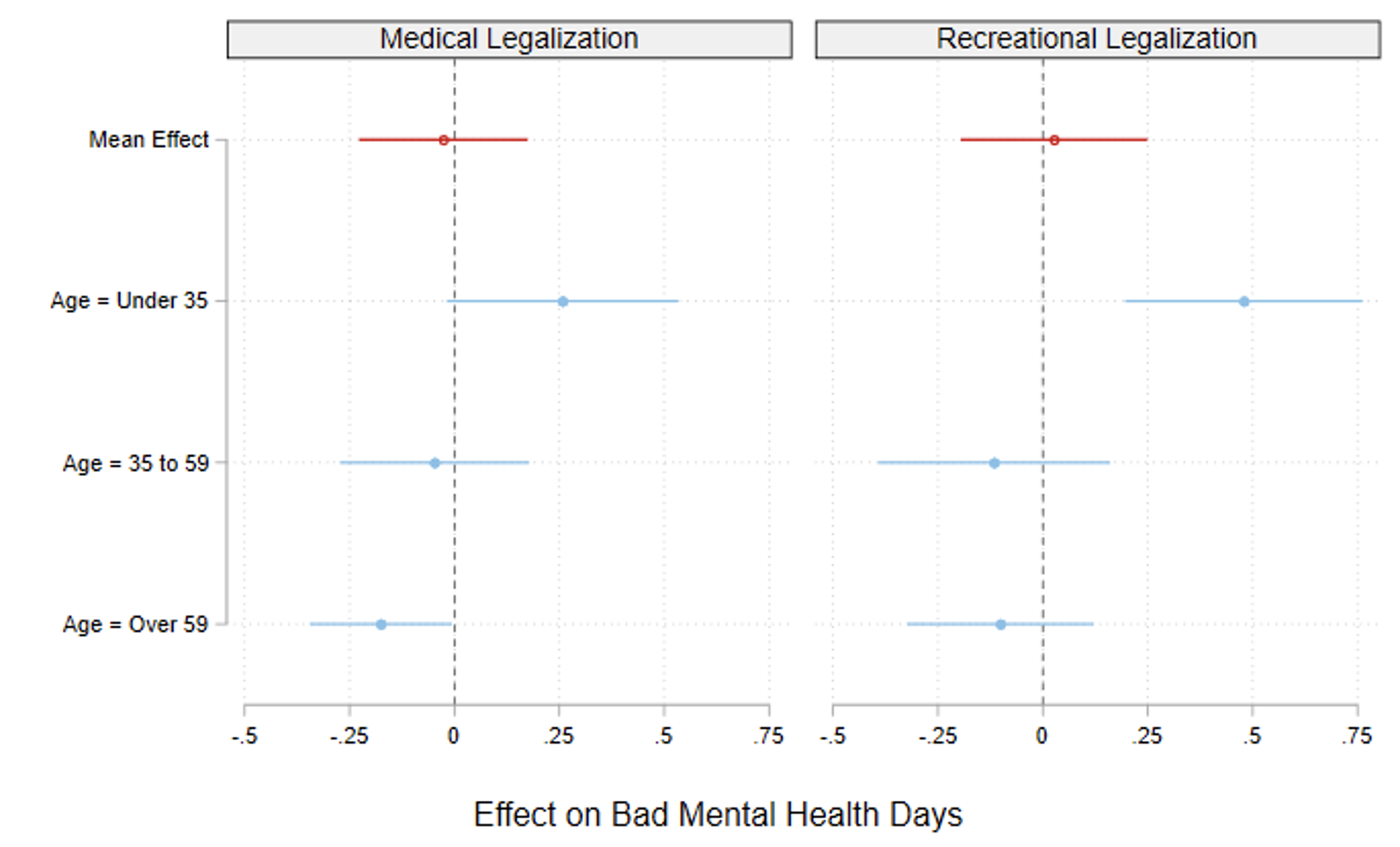
Our empirical analysis shows no evidence of an overall effect on mental health, and effects are consistent for both mental health measures, as shown in Figure 1, which reports the point estimate corresponding to the effect of legalising medical marijuana (left panel) and recreational marijuana (right panel) on days of bad mental health. This is despite finding a clear positive effect on marijuana use for both medical and recreational marijuana laws, with increasing long-run effects for MMLs. Nonetheless, the overall null effect masks sharp heterogeneities across the age distribution: while older age groups (over 59) seem to benefit from medical marijuana legalisation through reduced mental distress, recreational marijuana legalisation leads to increased mental distress for younger people (under 35), which is driven by the 18-25 group. Legalising medical marijuana reduces the number of days of bad mental health per year by almost a quarter of a day for older people, whereas for younger people legalising recreational marijuana increases the number of days of bad mental health per year by around half a day. The beneficial MML effects for the older age group are driven by those with pre-existing chronic health conditions, which we proxy with diagnosed diabetes, whereas for younger people, the adverse effects of RMLs are driven by relatively healthy individuals, with women being overall the most responsive. Our results are in line with an interpretation of positive mental health effects from MMLs likely due to the use of marijuana as a medical treatment of mental health distress associated with other chronic conditions, while the negative RMLs effects on younger people might be explained by overuse for recreational purposes.
Figure 1 Effect of medical and recreational legalisation on mental health
Notes: Each dot represents the point estimate corresponding to the effect of legalisation of medical (left panel) and recreational (right panel) marijuana, respectively, along with the 95% confident interval derived from our regression analysis. Red dots refer to full sample results, blue dots refer to the results by age groups.
Economic costs
Relying on a back-of-the-envelope calculation, we quantify the economic cost of the mental health effects of RMLs on young people to be about $184.2 per person per year. On the other hand, improvement in mental health for the older age group due to MMLs translates into a reduction in the economic costs of about $73.7 per person per year.
Overall, our results suggest that marijuana laws can have very different effects across age groups and type of legislation, with important implications for public policy and finances, as suggested by the negative (and unintended) public health consequences of legalising recreational marijuana on young and relatively healthy individuals.
References
Anderson, D M, D I Rees, and E Tekin (2018), “Medical marijuana laws and workplace fatalities in the United States”, International Journal of Drug Policy 6: 33–39.
Anderson, D M and D I Rees (forthcoming), “The Public Health Effects of Legalizing Marijuana”, Journal of Economic Literature.
Baggio, M, A Chong, and D Simon (2020), “Sex, marijuana and baby booms”, Journal of Health Economics 70, 102283.
Bambico, F R, N Katz, G Debonnel, and G Gobbi (2007), “Cannabinoids Elicit Antidepressant-Like Behavior and Activate Serotonergic Neurons through the Medial Prefrontal Cortex”, Journal of Neuroscience 27(43): 11700–11711.
Borbely, D, O Lenhart, J Norris, and A Romiti (2022), “Marijuana Legalization and Mental Health”, IZA Discussion Paper No. 15803.
Carpenter, C and C Dobkin (2009), “The Effect of Alcohol Consumption on Mortality: Regression Discontinuity Evidence from the Minimum Drinking Age”, American Economic Journal: Applied Economics 1(1): 164–82.
Chadwick, B, M L Miller, and Y L Hurd (2013), “Cannabis use during adolescent development: susceptibility to psychiatric illness”, Frontiers in Psychiatry 4: 129.
Chu, Y-W and W Townsend (2019), “Joint culpability: The effects of medical marijuana laws on crime”, Journal of Economic Behavior & Organization 159: 502–525.
Crost, B and S Guerrero (2012), “The effect of alcohol availability on marijuana use: Evidence from the minimum legal drinking age”, Journal of Health Economics 31(1): 112–121.
Dragone, D, G Prarolo, P Vanin, and G Zanella (2019), “Crime and the legalization of recreational marijuana”, Journal of Economic Behavior & Organization 159: 488–501.
Hansen, B, K Miller, and C Weber (2020), “Early evidence on recreational marijuana legalization and traffic fatalities”, Economic Inquiry 58(2): 547–568.
Hollingsworth, A, C Wing, and A C Bradford (2022), “Comparative Effects of Recreational and Medical Marijuana Laws on Drug Use among Adults and Adolescents”, The Journal of Law and Economics 65(3): 515–554.
Kelly, E and I Rasul (2014), “Policing cannabis and drug related hospital admissions: Evidence from administrative records”, Journal of Public Economics 112: 89–114.
National Academies et al. (2017), The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research.
Nicholas, L H and J C Maclean (2019), “The effect of medical marijuana laws on the health and labor supply of older adults: Evidence from the health and retirement study”, Journal of Policy Analysis and Management 38(2): 455–480.
van Ours, J C and A Palali (2013), “Easy access to cannabis is tempting”, VoxEU.org, 12 October.
Williams, J and J C van Ours (2009), “Cannabis use and mental health problems”, VoxEU.org, 19 September.