The COVID-19 pandemic inflicted enormous economic, social, and health costs (Agrawal et al. 2023, Cutler and Summers 2020, Viscusi 2023, Qiu et al. 2020, Chetty et al. 2020, Levy Yeyati and Filippini 2021). As of January 2024, approximately 7 million COVID-19 deaths have been reported globally.
Beyond the tremendous loss of life, the pandemic has affected many facets of life, including people’s jobs and incomes due to disruptions in economy, visits to healthcare providers, social life and outdoor activities, distress caused by social isolation, loss of loved ones, fear of job loss, risk of getting infected, learning loss due to school closures, and so on (Cantor et al. 2022, Whaley et al. 2020, Ziedan et al. 2020, Chetty et al. 2020, Breslau et al. 2021, Raviv et al. 2021, Ettman et al. 2020, Maisonneuve et al. 2023, Kenny et al. 2021, Guglielminetti et al. 2021).
In order to protect people from infection and avert pandemic catastrophe, the first COVID-19 vaccine was approved for use in the US by the Food and Drug Administration on 11 December 2020, which led to the launch of the global COVID-19 vaccination campaign. Prior studies have examined the impact of vaccines on COVID-19 deaths (Gupta et al. 2021, Steele et al. 2022, Haas et al. 2022, He et al. 2022, Watson et al. 2022). However, the impacts of the global COVID-19 vaccination campaign on worldwide all-cause mortality are not fully understood. While data from clinical trials suggest that vaccines are safe and effective (Polack et al. 2020, Baden et al. 2021, Voysey et al. 2021), they fail to capture the real-world effectiveness of COVID-19 vaccines in averting deaths for a variety of reasons. First, individuals in the real world might change protective behaviours in response to vaccinations compared to participants in clinical trials, as participants in clinical trials did not have evidence on the effectiveness of the vaccine and they were blind to whether they received the experimental vaccine or a placebo (Agrawal et al. 2022). Second, the effectiveness of vaccines might depend on the variant of infection. The dominant variants when vaccines underwent clinical trials were different than the variants that were widespread when vaccines were introduced (Katella 2023). Third, the effectiveness of the vaccines might depend on prior infection status, and most clinical trial participants did not have a prior infection. Fourth, the effectiveness of vaccines might reduce with time since vaccination due to wanning antibody levels (Tartof et al. 2021, Eyre et al. 2022, Menni et al. 2022, Ferdinands 2022). Fifth, COVID-19 vaccines might influence all-cause mortality by affecting mental health, social isolation, healthcare use, and economic activity (Agrawal et al. 2021, Díaz et al. 2023, Deb et al. 2022, Kwok et al. 2021, Tawk et al. 2021); and clinical trials were underpowered to estimate the effects of vaccines on all-cause mortality. Sixth, clinical trials are not suitable for estimating general equilibrium effects, such as the effects of vaccination on reduced transmission of disease.
We examine the real-world effectiveness of the global COVID-19 vaccination campaign on all-cause mortality using observational data. We focus on all-cause mortality as it accounts for both direct and indirect effects of the vaccines. It also mitigates the problem of measurement errors and incorrect reporting of COVID-19 deaths.
Estimated lives saved across 141 countries
To calculate the effect of the COVID-19 vaccination campaign on all-cause mortality, we require data on the actual number of deaths occurring after the rollout of COVID-19 vaccines, as well as the number of deaths that might have occurred in a counterfactual world in which vaccines were not available. The difference in mortality between these two scenarios – the real and the counterfactual – provides an estimate of the number of lives saved due to the COVID-19 vaccination campaign. Since we cannot observe deaths in the counterfactual world of no vaccines for countries that vaccinated their populations, we use two quasi-experimental approach to estimate the effect of the vaccination campaign on all-cause mortality across 141 countries.
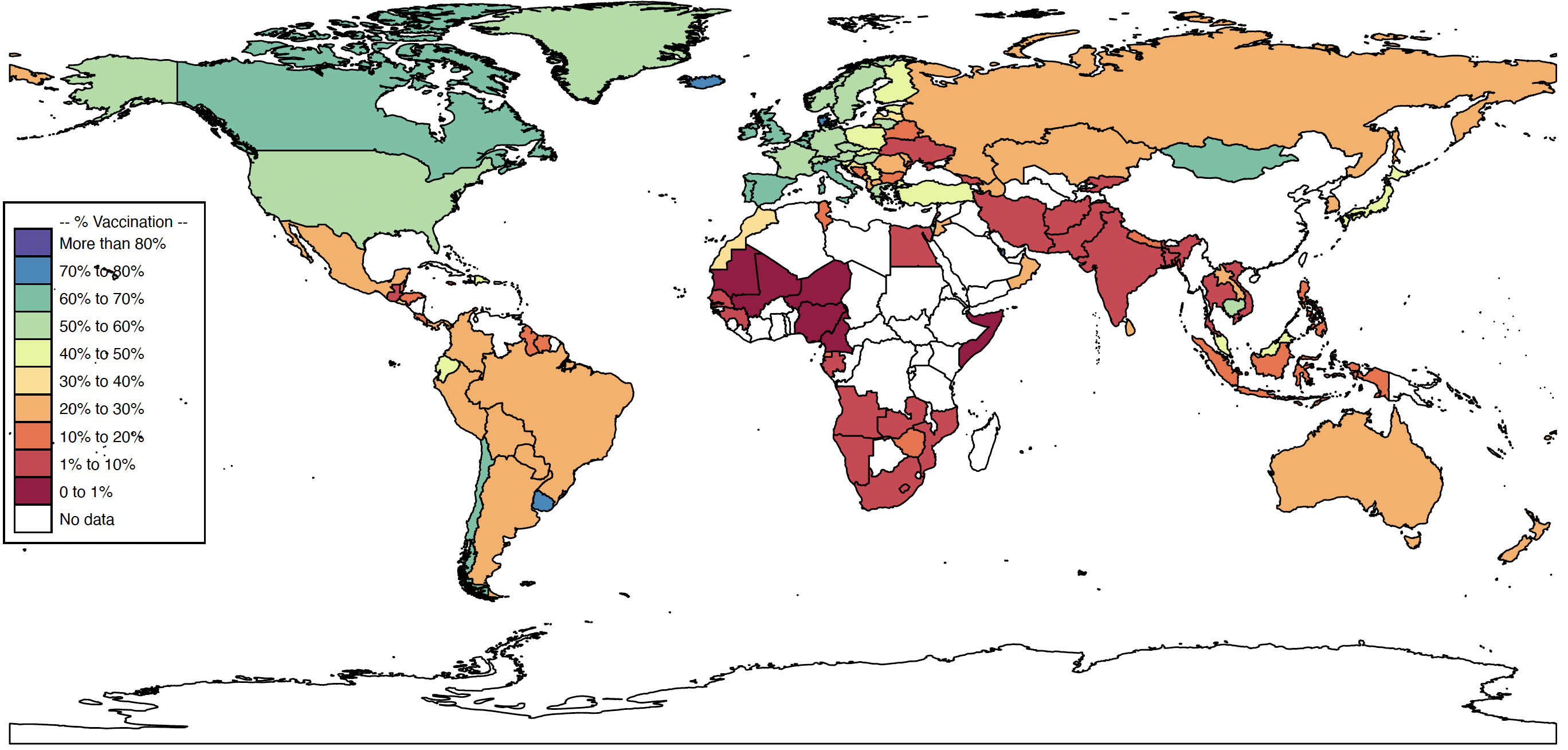
First, at the onset of COVID-19 vaccination campaign, vaccine availability varied across countries, resulting in some countries vaccinating their population earlier than others (see Figure 1). This staggered rollout of vaccines allows us to use the countries that were slow to vaccinate their population (control group) to predict deaths in countries that vaccinated their populations (treatment group) in the counterfactual world of vaccines not being available. For example, if by a certain date, country A had vaccinated 50% of their population but country B was yet to start its vaccination campaign, we can use data from Country B to predict what would have happened in Country A in the counterfactual world where country A also did not launch its vaccination campaign. Comparing deaths in the real world where country A vaccinated its population to the counterfactual world in which it did not provides an estimate of the lives saved by country A’s vaccination campaign. Doing this exercise for all countries that provided COVID-19 vaccines to their residents yields the total lives saved from the global vaccination campaign.
Figure 1 Worldwide share of population fully vaccinated by August 2021
Because the countries that did not administer COVID-19 vaccines might not be the ideal counterfactual for countries that did vaccinate their population, we used a second empirical approach to estimate the lives saved by COVID-19 vaccines globally. To do so, we use trends in all-cause mortality from the period when vaccines weren’t available to extrapolate or forecast deaths in the post vaccination period. Since we are using data from pre-vaccine availability period for the forecast, they provide an estimate of deaths in the counterfactual world of post vaccination period, in which vaccines were not available.
Using both the quasi-experimental approaches, we find that the COVID-19 vaccination campaign across 141 countries averted 2.4 million deaths by August 2021. We also calculate the value of lives saved using country and region-specific estimates of the value of statistical life (VSL) (Sweis 2022). We find that the lives saved during the first eight months of the COVID-19 vaccination campaign were valued at $6.5 trillion, which is approximately equal to 9% of the combined GDP of these 141 countries.
Equitable distribution
Finally, because the global distribution of vaccines has been uneven, with higher-income countries having earlier access to vaccines (Deb et al. 2023), we examine the potential impact of a more equitable counterfactual distribution of vaccines across 141 countries, where vaccination in each country is proportional to its population.
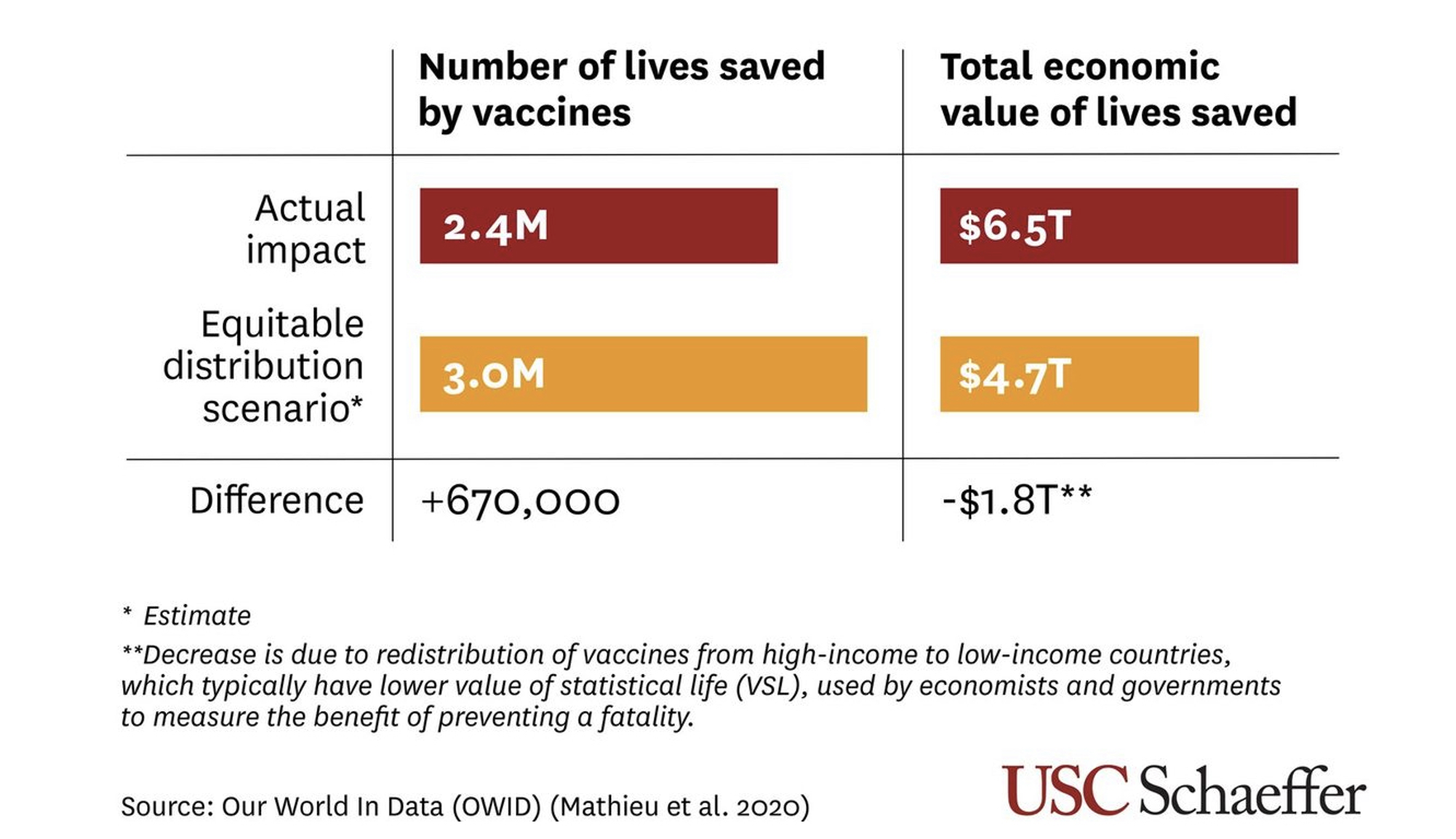
We estimate that with equitable distribution of vaccines among the 141 countries, the global COVID-19 vaccination campaign would have averted 670,000 more lives but with a $1.8 trillion decrease in the value of deaths averted (see Figure 2).
Figure 2 Change in lives saved and the value of lives saved (from actual to equitable distribution scenario)
This naturally raises the question: why does the value of lives saved decrease despite the increase in the number of lives saved with more equitable distribution? This happens because with a fixed supply of vaccines, a more equitable vaccine distribution implies reduced vaccination in richer countries and increased vaccination in poorer countries. It thus implies fewer lives saved in richer countries and more lives saved in poorer countries. Since VSL is positively correlated with per capita GDP, it is higher in richer countries compared to poorer countries. Therefore, we get the result that a more equitable distribution leads to lower value of lives saved. However, this does not mean that a more equitable distribution of vaccines is less desirable. VSL is just one metric for valuing lives, and it is likely not the best metric for comparing the value of lives across different countries. Considering the ethical view that all lives are equally important, a more equitable distribution would be more desirable as it would save more lives.
Conclusion
Our study contributes to the existing literature on the benefits of the global COVID-19 vaccination campaign by solving the limitations of clinical trials, and considering both direct and indirect effects of COVID-19 vaccines. The findings suggest that pharmaceutical interventions in the form of vaccination and therapeutics have a much larger protective effect on mortality compared to non-pharmaceutical interventions (NPIs), such as, shelter-in-place policies (Agrawal et al. 2023). Furthermore, our study adds to the literature on the most effective distribution strategy for ‘essential medicines’ during a global public health crisis. We find that the number of lives saved would have been much higher if vaccines were distributed more equitably.
References
Agrawal, V, J Cantor, N Sood, and C Whaley (2021), “The Impact of the COVID-19 Vaccine Distribution on Mental Health Outcomes”, NBER Working Paper w29593.
Agrawal, V, J Cantor, N Sood, and C Whaley (2023), “The Impact of COVID‐19 Shelter‐in‐place Policy Responses on Excess Mortality”, Health Economics, July, hec.4737.
Agrawal, V, N Sood, and C Whaley (2022), “The Ex-Ante Moral Hazard Effects of COVID-19 Vaccines”, NBER Working Paper w30602.
Baden, L R, H M El Sahly, B Essink et al. (2021), “Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine”, New England Journal of Medicine 384(5): 403–16.
Breslau, J, M L Finucane, A R Locker, M D Baird, E A Roth, and R L Collins (2021), “A Longitudinal Study of Psychological Distress in the United States before and during the COVID-19 Pandemic”, Preventive Medicine 143: 106362.
Cantor, J, N Sood, D M Bravata, M Pera, and C Whaley (2022), “The Impact of the COVID-19 Pandemic and Policy Response on Health Care Utilization: Evidence from County-Level Medical Claims and Cellphone Data”, Journal of Health Economics 82: 102581.
Chetty, R, J Friedman, N Hendren, M Stepner, and The Opportunity Insights Team (2020), “The Economic Impacts of COVID-19: Evidence from a New Public Database Built Using Private Sector Data”, NBER Working Paper w27431.
Cutler, D M, and L H Summers (2020), “The COVID-19 Pandemic and the $16 Trillion Virus”, JAMA 324(15): 1495–96.
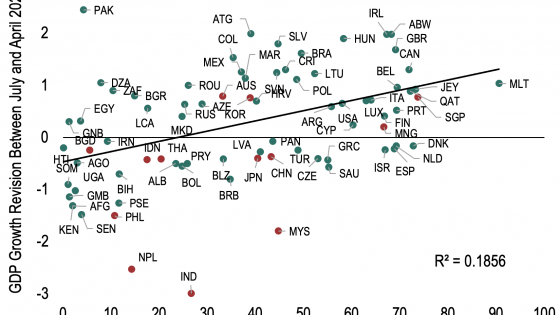
Deb, P, D Furceri, D Jimenez, S Kothari, J D Ostry, and N Tawk (2022), “The Effects of COVID-19 Vaccines on Economic Activity”, Swiss Journal of Economics and Statistics 158(1): 3.
Deb, P, D Furceri, D Jimenez, S Kothari, J D Ostry, and N Tawk (2023), “Determinants of COVID-19 Vaccine Rollouts and Their Effects on Health Outcomes”, Applied Health Economics and Health Policy 21(1): 71–89.
de La Maisonneuve, C, B Égert, and D Turner (2023), “Quantifying the Macroeconomic Impact of COVID-19-Related School Closures on Human Capital”, VoxEU.org, 24 January.
Díaz, F, P A Henríquez, N Hardy, and D Ponce (2023), “Population Well-Being and the COVID-19 Vaccination Program in Chile: Evidence from Google Trends”, Public Health 219: 22–30.
Ettman, C K, S M Abdalla, G H Cohen, L Sampson, P M Vivier, and S Galea (2020), “Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic”, JAMA Network Open 3(9): e2019686.
Eyre, D W, D Taylor, M Purver, D Chapman, T Fowler, K B Pouwels, A S Walker, and T E A Peto (2022), “Effect of Covid-19 Vaccination on Transmission of Alpha and Delta Variants”, New England Journal of Medicine 386(8): 744–56.
Ferdinands, J M (2022), “Waning 2-Dose and 3-Dose Effectiveness of mRNA Vaccines Against COVID-19–Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance — VISION Network, 10 States, August 2021–January 2022”, MMWR. Morbidity and Mortality Weekly Report 71.
Guglielminetti, E, C Rondinelli, and V Ercolani (2021), “Fears for the Future: Saving Dynamics after the Covid-19 Outbreak”, VoxEU.org, 26 June.
Gupta, S, J Cantor, K I Simon, A I Bento, C Wing, and C M Whaley (2021), “Vaccinations Against COVID-19 May Have Averted Up To 140,000 Deaths In The United States”, Health Affairs 40(9): 1465–72.
Haas, E J, J M McLaughlin, F Khan et al. (2022), “Infections, Hospitalisations, and Deaths Averted via a Nationwide Vaccination Campaign Using the Pfizer–BioNTech BNT162b2 mRNA COVID-19 Vaccine in Israel: A Retrospective Surveillance Study”, The Lancet Infectious Diseases 22(3): 357–66.
He, D, S T Ali, G Fan, D Gao, H Song, Y Lou, S Zhao, B J Cowling, and L Stone (2022), “Evaluation of Effectiveness of Global COVID-19 Vaccination Campaign”, Emerging Infectious Diseases 28(9): 1873–76.
Katella, K (2023), “Omicron, Delta, Alpha, and More: What To Know About the Coronavirus Variants”, Yale Medicine, 3 February.
Kenny, G, D Georgarakos, T Jappelli, and D Christelis (2021), “Heterogenous Effects of Covid-19 on Households’ Financial Situation and Consumption: Cross-Country Evidence from a New Survey”, VoxEU.org, 8 June.
Kwok, K O, K-K Li, W I Wei, A Tang, S Y S Wong, and S S Lee (2021), “Influenza Vaccine Uptake, COVID-19 Vaccination Intention and Vaccine Hesitancy among Nurses: A Survey”, International Journal of Nursing Studies 114: 103854.
Levy Yeyati, E, and F Filippini (2021), “Pandemic Divergence: The Social and Economic Costs of Covid-19”, VoxEU.org, 12 May.
Menni, C, A May, L Polidori et al. (2022), “COVID-19 Vaccine Waning and Effectiveness and Side-Effects of Boosters: A Prospective Community Study from the ZOE COVID Study”, The Lancet Infectious Diseases 22(7): 1002–10.
Polack, F P, S J Thomas, N Kitchin et al. (2020), “Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine”, New England Journal of Medicine 383(27): 2603–15.
Qiu, R T R, J Park, S Li, and H Song (2020), “Social Costs of Tourism during the COVID-19 Pandemic”, Annals of Tourism Research 84: 102994.
Raviv, T, C M Warren, J J Washburn et al. (2021), “Caregiver Perceptions of Children’s Psychological Well-Being During the COVID-19 Pandemic”, JAMA Network Open 4(4): e2111103.
Steele, M K, A Couture, C Reed et al. (2022), “Estimated Number of COVID-19 Infections, Hospitalizations, and Deaths Prevented Among Vaccinated Persons in the US, December 2020 to September 2021”, JAMA Network Open 5(7): e2220385.
Sweis, N J (2022), “Revisiting the Value of a Statistical Life: An International Approach during COVID-19”, Risk Management 24(3): 259–72.
Tartof, S Y, J M Slezak, H Fischer et al. (2021), “Effectiveness of mRNA BNT162b2 COVID-19 Vaccine up to 6 Months in a Large Integrated Health System in the USA: A Retrospective Cohort Study”, Lancet (London, England) 398(10309): 1407–16.
Tawk, N, J D Ostry, S Kothari, D Jiménez, D Furceri, and P Deb (2021), “The Economic Effects of COVID-19 Vaccines”, VoxEU.org, 16 December.
Viscusi, W K (2023), “The Global COVID-19 Mortality Cost Report Card: 2020, 2021, and 2022”, PloS One 18(5): e0284273.
Voysey, M, S A Costa Clemens, S A Madhi et al. (2021), “Safety and Efficacy of the ChAdOx1 nCoV-19 Vaccine (AZD1222) against SARS-CoV-2: An Interim Analysis of Four Randomised Controlled Trials in Brazil, South Africa, and the UK”, The Lancet 397(10269): 99–111.
Watson, O J, G Barnsley, J Toor, A B Hogan, P Winskill, and A C Ghani (2022), “Global Impact of the First Year of COVID-19 Vaccination: A Mathematical Modelling Study”, The Lancet Infectious Diseases 22(9): 1293–1302.
Whaley, C M, M F Pera, J Cantor et al. (2020), “Changes in Health Services Use Among Commercially Insured US Populations During the COVID-19 Pandemic”, JAMA Network Open 3(11): e2024984.
Ziedan, E, K Simon, and C Wing (2020), “Effects of State COVID-19 Closure Policy on NON-COVID-19 Health Care Utilization”, NBER Working Paper w27621.