Economic research and policy debate about the minimum wage has focused on economic outcomes, most notably employment and earnings of low-skilled workers and incomes and poverty. Research has established both pros and cons of higher minimum wages: higher wages for some but – according to most research – job loss for others, and unclear benefits for low-income families in general. For this reason, perhaps, minimum wage policy in the US remains at an impasse. Some states (and localities) have opted for much higher minimum wages, while the federal minimum wage of $7.25, which has not increased since 2009, remains binding in 20 states.
In recent years, researchers have turned to the effects on a multitude of other behaviours and outcomes – mostly health-related. Some studies have led to headlines touting the effects of higher minimum wages in reducing suicides, decreasing smoking, increasing birthweights, lowering depression, improving diet, combatting child neglect, and more (e.g. Cherkis 2021, Gardner 2016, National Employment Law Project 2021, Desmond 2019). If a higher minimum wage delivers these kinds of benefits, then perhaps this evidence should weigh more heavily in the policy debate, offsetting the evidence of job loss from higher minimum wages, and instead supporting substantial increases in the minimum wage.
Advocacy for higher minimum wages based on health benefits
Indeed, findings like these have led influential health research and advocacy organisations to recommend minimum wage increases to improve health. The American Public Health Association advocates raising and regularly updating the federal minimum wage: “More than a decade’s worth of research indicates that increasing the minimum wage is an effective means of improving public health across many settings” (American Public Health Association 2016). The statement cites evidence, for example, that higher minimum wages reduce premature deaths among adults. Similarly, the American Medical Association has endorsed increases in federal, state, and local minimum wages, citing studies finding that higher minimum wages reduce low-weight births and neonatal deaths (American Medical Association 2022).
What does economics predict?
The potential for higher minimum wages to improve health is clear, via raising incomes for some workers (and their families), which can increase expenditures of time and money on health-promoting goods and services and reduce financial stress. On the other hand, job loss can reduce income among other workers and their families, with the opposite effects. The American Public Health Association discounts the latter possibility, citing very selectively from research on employment effects to argue that “recent research has shown that minimum wage increases have very little effect….” In contrast, most studies of minimum wages and health acknowledge these offsetting influences (e.g. Andreyeva and Ukert 2018, Horn et al. 2017, Wehby et al. 2020).
Nonetheless, health benefits from income gains for some workers could outweigh adverse health effects for others who lose their jobs, especially given that there are almost certainly more income gainers than job losers. A net gain would be more likely if there was clear evidence that minimum wages raise incomes in lower-income families. However, the evidence on family income is ambiguous, in part because many minimum-wage workers are not in poor or low-income families, and many low-income families have no workers.
In fact, the predictions of the Grossman (1972) model for health are unclear. We face a diverse set of choices about spending and the allocation of time that can affect health, including purchasing healthcare (physical as well as mental), exercise, diet, goods consumption, and more. Even if the positive effects of minimum wages on income predominate job-loss effects, these choices can be affected in varying ways with different implications for health, depending on the income elasticity of demand for health-related expenditures of money (and time), and the substitutability of health-related goods and activities with time allocated to the labour market (which can be influenced by minimum wages).
Conclusions about how minimum wages impact health and related behaviours or outcomes require careful weighing of the evidence. It also requires recognition that the effects may vary for different behaviours or outcomes because of variation in the sensitivity of health-related expenditures and activities to income and time allocation. Additionally, there is heterogeneity in this sensitivity for workers differentially affected by higher minimum wages.
Assessing the evidence
Given these considerations, it is perhaps not surprising that the evidence on the effects of minimum wages on health and related behaviours or outcomes is more nuanced than the American Public Health Association and American Medical Association statements indicate. Many studies in this recent literature fail to find beneficial health (or related) effects, and some find negative effects. In addition, some studies find effects that might seem surprisingly large or unexpected – like 8,000 fewer suicides nationally from a $1 increase in the minimum wage (Gertner et al. 2019) or reduced heart disease deaths for 35–64 year-olds (Van Dyke et al. 2018).
This raises the possibility that researchers, as well as policy advocates, are sometimes drawing conclusions that are driven more by spurious changes in minimum wages and in health or related behaviours than by causal effects of changes in minimum wage.
In a recent working paper (Neumark 2023), I assess this emerging body of evidence on minimum-wage effects on health and health-related behaviours, including some dimensions of ‘risky’ behaviour. In addition to assessing the individual studies, I try to determine the conclusions we can draw from studies that use more convincing research designs.
The research I survey covers nine categories of health and related behaviours:
- adult and teen health
- infant and child health
- diet and obesity
- mental health
- suicide (a specific subset of mental health)
- family structure and children
- risky behaviour
- crime
- mechanisms that can affect health (like health insurance).
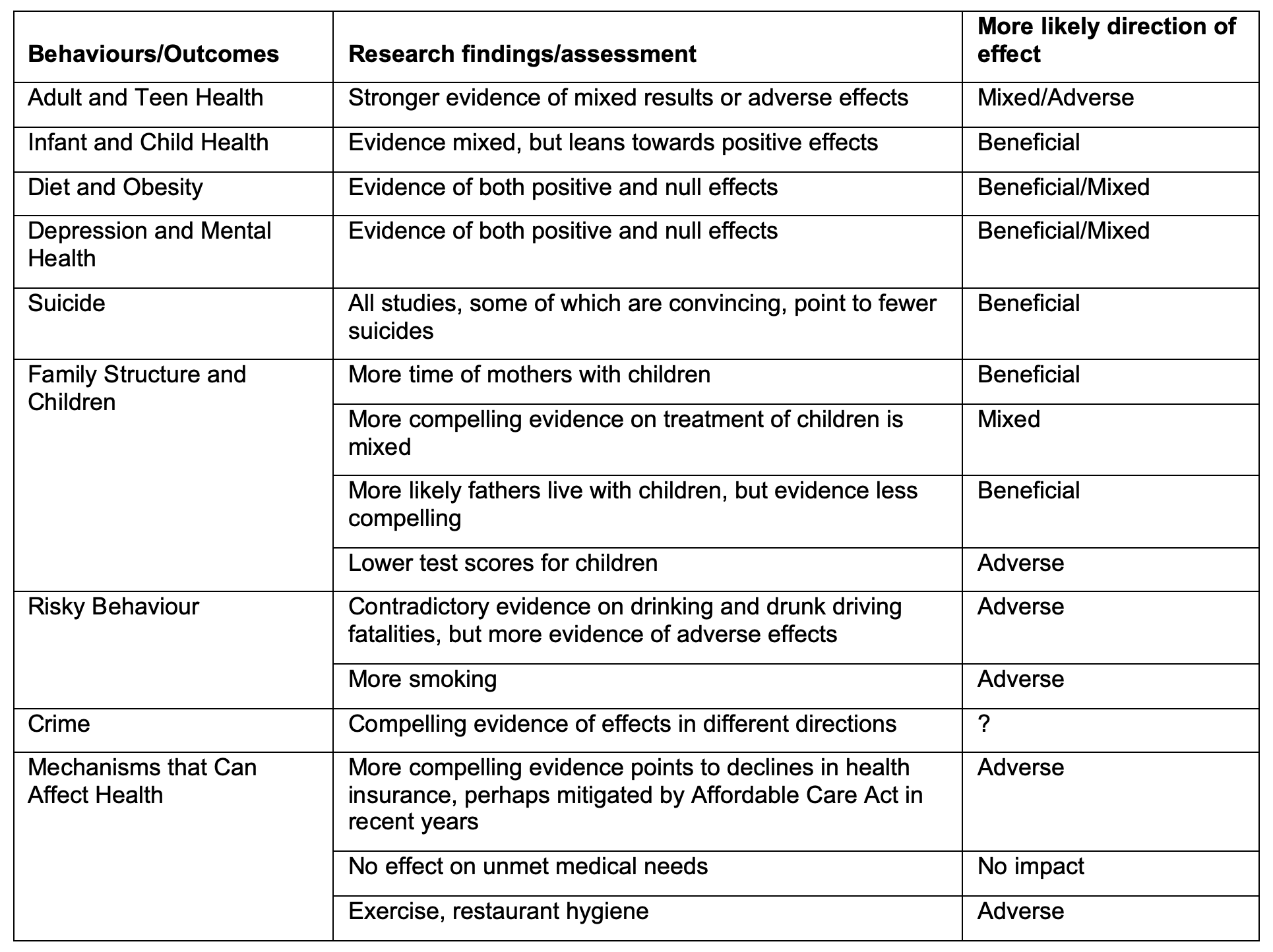
Looking across these categories of health behaviours or outcomes, it is not possible to draw conclusions that point unambiguously in one direction or the other, although within these categories one can more readily draw some conclusions. The evidence across the 63 papers covered in the survey is summarised briefly in Table 1. Detailed tables in the working paper discuss each study, organised by these nine dimensions of health.
Table 1 Summary table on minimum wage effects
The evidence on overall physical health is clearly mixed (e.g. Lebihan 2022, Averett et al. 2018, Buszkiewicz et al. 2021), although a number of the studies claiming beneficial effects are less convincing. This ambiguity may reflect the conflicting evidence on factors that can affect health in some of the other analyses I consider. The findings on minimum-wage effects on diet and obesity either point to beneficial effects (Palazzolo and Pattabhiramaiah 2021) or null effects (e.g. Chapman et al. 2021), but not negative effects. Other evidence indicates that higher minimum wages increase smoking (Huang et al. 2021) and reduce exercise (Lenhart 2019) and possibly hygiene (Chakrabarti et al. 2021).
The evidence for mental health is ambiguous. There are somewhat more studies finding no impact (e.g. Kronenberg et al. 2017) than finding a positive impact (Bai and Veall 2023); none find a negative impact. And, perhaps surprisingly, the evidence for suicide points only to beneficial effects of higher minimum wages (e.g. Dow et al. 2020).
Moving further away from traditional health behaviours and outcomes, studies on family structure and children point in different directions, with evidence that mothers spend more time with children (Gearhart et al. forthcoming), no clear indication of changes in treatment of children (Ash et al. forthcoming), but declines in children’s test scores (Regmi 2020). The evidence generally points to minimum wages increasing risky behaviour – mainly drinking and smoking (e.g. Hoke and Cotti 2016). Evidence on the effects of minimum wages on crime is mixed (e.g. Agan and Makowsky forthcoming, versus Fone et al. 2023).
The best evidence on employer-provided health insurance is more adverse (e.g. Marks 2011), although Medicaid expansions under the Affordable Care Act may have mitigated this influence, and there is no clear evidence of greater unmet medical needs when minimum wages increase (Sabia and Nielsen 2015). And as noted above, other evidence suggests that higher minimum wages may affect health adversely via different channels.
Conclusions
Overall, the mixed conclusions on how minimum wages affect health and related behaviours undermine the evidence base for concluding that “the minimum wage is an effective means of improving public health across many settings” (American Public Health Association 2016).
This survey also points to lessons for research. Many studies of the effects of minimum wages on health and related behaviours fall well short of the rigour that characterises more recent research in labour economics on the employment effects of minimum wages. It seems likely that more rigorous types of evaluations will come to the research on minimum wages and health – and indeed there are already examples, like the work of Dow et al. (2020) on suicides. Whether this leads to less ambiguous conclusions or just reinforces the potentially conflicting effects predicted by theoretical modelling of how minimum wages can affect health remains to be seen.
References
Agan, A Y, and M D Makowsky (forthcoming), “The minimum wage, EITC, and criminal recidivism”, Journal of Human Resources.
American Medical Association (2022), “AMA adopts new policy connecting poverty-level wages to adverse health”, American Medical Association, 13 June.
Andreyeva, E, and B Ukert (2018), “The impact of the minimum wage on health”, International Journal of Health Economics and Management 18: 337–75.
American Public Health Association (2016), “Improving health by increasing the minimum wage”, APHA Policy Statement, 1 November.
Ash, M J, et al. (forthcoming), “The impact of increased minimum wage on child neglect varies by developmental age of child”, Journal of Interpersonal Violence.
Averett, S L, J K Smith, and Y Wang (2018), “Minimum wages and the health of Hispanic women”, Journal of Economics, Race, and Policy 1: 217–39.
Bai, Y, and M R, Veall (2023), “Minimum wages and mental health”, SSM-Mental Health 3: 100187.
Baskaya, Y S, and Y Rubinstein (2015), “Using Federal minimum wages to identify the impact of minimum wages on employment and earnings across US states”, Central Bank of Turkey.
Buszkiewicz, J H, H D Hill, and J J Otten (2021), “Association of state minimum wage rates and health in working-age adults using the National Health Interview Survey”, American Journal of Epidemiology 190: 21–30.
Card, D, and A B Krueger (1994), “Minimum wages and employment: A case study of the fast-food industry in New Jersey and Pennsylvania”, American Economic Review 84: 772–93.
Chakrabarti, S K, S Devaraj, and P C Patel (2021), “Minimum wage and restaurant hygiene violations: Evidence from Seattle”, Managerial and Decision Economics 42: 85–99.
Chapman, L E, et al. (2021), “Association between hourly wages and dietary intake after the first phase of implementation of the Minneapolis Minimum Wage Ordinance”, Public Health Nutrition 24: 3552–65.
Cherkis, J (2021), “What happens to your mental health when you can’t pay your rent?”, New York Times, 10 March.
Clemens, J, and M Wither (2019), “The minimum wage and the Great Recession: Evidence of effects on the employment and income trajectories of low-skilled workers”, Journal of Public Economics 170: 53–67.
Dow, W H, A Godøy, C Lowenstein, and M Reich (2020), “Can labor market policies reduce deaths of despair?”, Journal of Health Economics 74: 102372.
Dube, A, T W Lester, and M Reich (2010), “Minimum wage effects across state borders: Estimates using contiguous counties”, Review of Economics and Statistics 92: 945–64.
Fone, Z S, J J Sabia, and R Cesur (2023), “The unintended effects of minimum wage increases on crime”, Journal of Public Economics 219: 104780.
Gardner, B (2016), “How to improve mental health in America: Raise the minimum wage”, New Republic, 4 May.
Gearhart, R, L Sonchak-Ardan, and R Thibault (forthcoming), “The impact of minimum wage on parental time allocation to children: Evidence from the American Time Use Survey”, Review of Economics of the Household.
Gertner, A K, J S Rotter, and P R Shafer (2019), “Association between state minimum wages and suicide rates in the US”, American Journal of Preventive Medicine 56: 648–54.
Grossman, M (1972), “On the concept of health capital and the demand for health”, Journal of Political Economy 80: 223–55.
Hoke, O, and C Cotti (2016), “Minimum wages and youth binge drinking”, Empirical Economics 51: 363–81.
Horn, B P, J C MacLean, and M R Strain (2017), “Do minimum wage increases influence worker health?” Economic Inquiry 55: 1986–2007.
Huang, C, F Liu, and S You (2021), “The impact of minimum wage increases on cigarette smoking”, Health Economics 30: 2063–91.
Jha, P, D Neumark, and A Rodriguez-Lopez (2022), “What’s across the border? Re-evaluating the cross-border evidence on minimum wage effects”, IZA Discussion Paper 15282.
Kaestner, R, G Wehby, and D Dave (2016), “The impact of minimum wage changes on infant health”, VoxEU.org, 26 September.
Kronenberg, C, R Jacobs, and E Zucchelli (2017), “The impact of the UK national minimum wage on mental health”, SSM-Population Health 3: 749–55.
Lebihan, L (2022), “Minimum wages and health: Evidence from European countries”, International Journal of Health Economics and Management 23: 85–107.
Lenhart, O (2019), “Higher wages, less gym time? The effects of minimum wages on time use”, Southern Economic Journal 86: 253–70.
Marks, M (2011), “Minimum wages, employer-provided health insurance, and the non-discrimination law”, Industrial Relations 50: 241–62.
National Employment Law Project (2021), “Why the US needs a $15 minimum wage”, NELP Fact Sheet, 26 January.
Neumark, D (2023), “The effects of minimum wages on (almost) everything? A review of recent evidence on health and related behaviors”, NBER Working Paper 31191.
Neumark, D, J M I Salas, and W Wascher (2014), “Revisiting the minimum wage-employment debate: Throwing out the baby with the bathwater?” ILR Review 67(Supp.): 608–48.
Palazzolo, M, and A Pattabhiramaiah (2021), “The minimum wage and consumer nutrition”, Journal of Marketing Research 58: 845–69.
Regmi, K (2020), “The effect of the minimum wage on children’s cognitive achievement”, Labour Economics 65: 101844.
Sabia, J A, and R B Nielsen (2015), “Minimum wages, poverty, and material hardship: New evidence from the SIPP”, Review of Economics of the Household 13: 95–124.
Van Dyke, M E, et al. (2018), “State-level minimum wage and heart disease death rates in the US, 1980–2015: A novel application of marginal structural modeling”, Preventive Medicine 112: 97–103.
Wehby, G L, D M Dave, and R Kaestner (2020), “Effects of the minimum wage on infant health”, Journal of Policy Analysis and Management 39: 411–43.