Hospital mergers are a ubiquitous and ongoing phenomenon across US healthcare markets. Nearly 1,600 hospital mergers took place from 1998 to 2017 (Gaynor 2020). Mergers are a key topic of study because they influence competition, which has an outsize role in the quality of care received by patients (Gaynor and Propper 2010, Gobillon and Milcent 2017). The general consensus of the research is that hospital mergers increase prices for both patients and insurers without measurable gains in clinical quality of care or other improvements (e.g. Gowrisankaran et al. 2015, Tenn 2011, Beaulieu et al. 2020, Capps 2005). However, the literature offers less evidence about the mechanisms through which mergers affect (or fail to affect) clinical and financial outcomes.
In a new study, we examine the organisational mechanisms that drive merger effects in the context of a particularly large and consequential hospital acquisition (Gaynor et al. 2021). This setting is ideal to ‘open the black box’ of hospital mergers. This mega-merger involved two of the largest for-profit chains in the US, comprising over 100 individual hospitals, making it important in its own right. But focusing on a single merger has the additional benefit of letting us look closely at the claims of the acquiring chain about how it would improve performance at its targets – and whether those claims were realised. We also have a unique window into this merger because we conducted management surveys of executives at many of the hospitals in the chain (Bloom et al. 2010). These surveys helped us see further into the organisation’s operations than much of the past literature.
Our new work shows that improving hospital performance through mergers is difficult. Even though the acquirer firm in the mega-merger we study had a great deal of experience growing by purchasing other hospitals, they failed to improve financial or patient outcomes at their targets. The merger led to changes in the target hospitals’ leadership, management practices, and IT systems. However, despite clear signs of these changes in the hospital production process in the data, the hoped-for improvements in outcomes did not materialise. For most of our analyses, we looked at changes from before to after the merger in three sets of hospitals: the target facilities that were purchased, the legacy acquirer facilities that were already a part of the chain, and other for-profit hospitals. We used the other hospitals as a control group in the analyses.
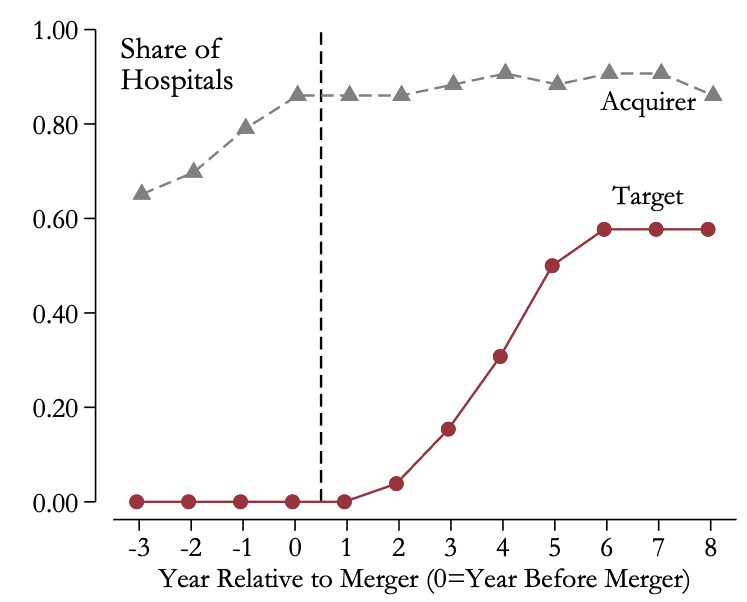
We found that the merger did lead to a few changes in the production process and organisation at target hospitals, in some cases achieving the changes the acquirer claimed it would make prior to the merger. For instance, the acquirer said it would achieve cost savings by standardising operations across the hospitals, and we see some signs of success on that front when we look at hospitals’ use of health information technology. The target hospitals successfully harmonised their electronic medical record (EMR) systems with the acquirer’s. Here, the patterns are striking. At the time of the merger, none of the target hospitals was using the acquirer’s EMR. Within five years of the merger, however, three-fifths of the target hospitals adopted the acquirer’s system (Figure 1). We also found that a similar share de-adopted a vendor they (uniquely) used before the merger.
Figure 1 Adoption rate of the acquiring chain’s EMR
The acquirer aimed to expand patient volume through an aggressive physician recruitment programme that they had deployed in their own hospitals in previous years. We examined this claim by tracking the arrival and departure of physicians at hospitals using hospitalisation data from Medicare (the national US health insurance programme). There were no significant effects of the merger on physician flows for acquirer or target hospitals. We also considered whether the acquisition led to changes in other inputs to the hospital production process like employment and capital investment. Here, we found some signs that the merger changed production: hospitals already in the acquirer chain cut their employment, while target hospitals cut their capital investment.
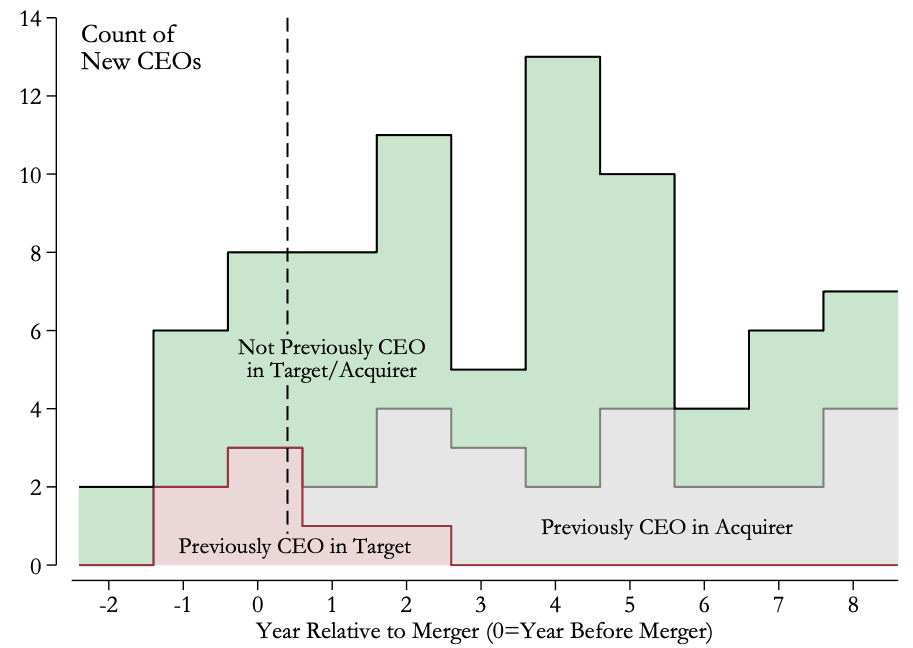
We next examined whether the acquisition affected where the hospitals sourced their managers. We used hospital survey data to track the work histories of their CEOs in the years leading up to their arrivals. This effort uncovered a striking shift at target hospitals after the merger. Previously, their new CEOs had arrived after working at other target hospitals or at hospitals outside the chain entirely; in some cases, they had not previously worked as a hospital CEO at all. However, after the acquisition, we found an influx of CEOs that previously held this position at a hospital in the acquiring chain (Figure 2). In many other cases, the new CEOs had worked at another lower-level role in the acquiring chain. In short, we found clear signs that the acquirer sought to influence the management of target facilities by sending its managers to the facilities it had taken over.
Figure 2 Origins of new CEOs at target hospitals
To examine how changes in leadership affected managerial practices, we surveyed the chain’s top managers in 2015 using the World Management Survey instrument. This survey measures the adoption of basic managerial practices and is applicable to a host of organisations including hospitals (Bloom et al. 2020). Managers were asked about 20 different practices and were scored from one to five, with higher values indicating closer adherence to best practices. We aggregated these scores to produce one overall management score for each hospital. As a point of comparison, we also considered management scores for hospitals in other chains, collected using the same instrument in an earlier study (Bloom et al. 2012). Three major patterns emerged from our analyses. First, we found that hospitals in the merged chain had significantly lower management scores relative to hospitals belonging to other chains. Second, variation in the management scores in the merged chain was lower than in other chains. Third, the acquirer hospitals and target hospitals looked quite similar in terms of average scores and degree of variation in the scores. These findings suggest that the merger led to the adoption of fairly uniform, albeit perhaps lower-quality, management practices within the chain.
Lastly, we turned to the merger’s effects on hospital performance. We investigated the effects on financial performance by focusing on the hospitals’ costs, prices, and profit margins. We found that the merger raised costs per hospitalisation at acquirer hospitals, yet had no detectable impact on costs at target facilities. Consistent with the previous literature, we found that the merger significantly increased hospital prices. And while revenues per hospitalisation rose significantly at acquirer facilities, we did not find a significant change at target hospitals. Bringing these findings together reveals that in spite of the post-merger price increases, cost growth outpaced growth in revenues. As a consequence, the profit margins at both acquirer and target hospitals failed to grow post-merger. Moreover, we found that profits at the acquirer’s legacy hospitals fell significantly.
To investigate clinical performance, we looked at the survival and readmission rates of Medicare patients. We assembled four groups of patients based on the main reason they came to the hospital: heart attack, heart failure, pneumonia, and stroke. We found no indication of post-merger improvements in survival outcomes at acquirer or target hospitals relative to other for-profit hospitals. A modest decline in readmission rates in acquirer hospitals was the one beneficial result (financial or clinical) of the merger we found. It is also worth noting that survival rates at these hospitals declined by a similar amount, enough to essentially offset the readmission improvements, although that change wasn’t statistically significant. Putting these results together, it would be hard to interpret them as indicative of broader success.
Overall, our study builds on the prior literature by zooming in on a large hospital chain merger. With this approach, we were able to gain deeper insight into the effects of mergers and the forces that drive them. We found evidence that the acquirer sought to influence the hospital production process by making investments in health information technology and bringing in its own managers. Yet there was little evidence that these efforts improved performance. Here we note a key puzzle: the organisation we study was financially motivated to improve, yet the merger led to no clear performance gains at the hospitals that were purchased. This result suggests that of all the levers it could move to raise performance, the chain exerted its strongest influence on the levers that were easiest to implement but delivered little payoff: it shuffled CEOs and purchased new medical record systems.
We think our findings offer important lessons for merger policy (Crawford and Caffara 2021, Nocke and Whinston 2021). They demonstrate the value of taking an organisational view to evaluating whether a merger is likely to achieve hoped-for efficiencies. An approach that considers the acquirers’ stated aims, how firms intend to implement these aims inside their own organisations, and whether these changes are likely to drive performance improvements could help regulators assess the likelihood that claimed efficiencies will actually be realised. This method may help identify ‘good mergers’ in which efficiencies offset the harms of reduced competition (Ashenfelter and Hosken 2008, Dafny and Lee 2015). In our study, an evaluation of the acquirer’s stated aims may have raised doubts that the acquirer’s approach to the merger – through investments in IT investments and new managerial personnel – would improve quality or profits.
References
Ashenfelter, O and D Hosken (2008), “The effect of mergers on consumer prices: evidence from five selected case studies”, VoxEU.org, 22 April.
Beaulieu, N D, L S Dafny, B E Landon, J B Dalton, I Kuye and J M McWilliams (2020), “Changes in Quality of Care after Hospital Mergers and Acquisitions”, New England Journal of Medicine 382, 51–59.
Bloom, B, R Homkes, R Sadun and J Van Reenen (2010), “Why good practices really matter in healthcare”, VoxEU.org, 17 December.
Bloom, N, C Genakos, R Sadun and J Van Reenen (2012), “Management practices across firms and countries”, Academy of Management Perspectives 26, 12–33.
Bloom, N, R Lemos, R Sadun and J Van Reenen (2020), “Healthy Business? Managerial Education and Management in Health Care”, Review of Economics and Statistics 102, 506–517.
Bloom, N and J Van Reenen (2007), “Measuring and Explaining Management Practices Across Firms and Countries”, The Quarterly Journal of Economics 122, 1351–1408.
Capps, C (2005), “The quality effects of hospital mergers”, Discussion paper, U.S. Department of Justice, Antitrust Division.
Crawford, G and C Caffara (2021), “Turning competition research into competition policy”, VoxEU.org, 08 June.
Dafny, L S and T H Lee (2015), “The Good Merger”, New England Journal of Medicine 372, 2077–2079.
Gaynor, M (2020), “What to Do about Health-Care Markets? Policies to Make Health-Care Markets Work”, Policy Proposal No. 2020–10, The Hamilton Project.
Gaynor, M and C Propper (2010), “Healthcare competition saves lives”, VoxEU.org, 23 August.
Gobillon, L and C Milcent (2017), “The effects of decentralisation and competition on hospital management and performance in France”, VoxEU.org, 21 July.
Gowrisankaran, G, A Nevo and R Town (2015), “Mergers When Prices Are Negotiated: Evidence from the Hospital Industry”, American Economic Review 105, 172–203.
Nocke, V and M Whinston (2020), “On concentration screens in horizontal merger review”, VoxEU.org, 26 August.
Tenn, S (2011), “The Price Effects of Hospital Mergers: A Case Study of the Sutter–Summit Transaction”, International Journal of the Economics of Business 18, 65–82.